Understanding Cellular Dysfunction: Causes & Effects
The intricate machinery within our cells is exquisitely designed to sustain life, but when this machinery falters, the phenomenon known as cellular dysfunction arises. This disruption can have far-reaching implications for our health, laying the groundwork for widespread cell damage and disease. While the resilience of our bodies often manages to repair such impairments, the journey of understanding and combating cell dysfunction remains a pivotal chapter in modern medicine.
Genetic anomalies, harmful environmental exposures, and the relentless wear and tear of aging contribute to cell dysfunction. These factors interfere with the cells’ innate repair mechanisms, slowing down the process of cell repair and regeneration. Recognizing these elements not only provides insight into the etiology of various conditions but also guides the development of strategies to fortify cellular health.
Exploring the Basis of Cellular Dysfunction
The core of cellular health lies in the well-orchestrated operations of various cell types, each playing its quintessential role. Among these, the vascular endothelium stands out as a critical component responsible for maintaining cellular function and integrity. As the innermost lining of our blood vessels, the endothelium acts as a gatekeeper, controlling the exchange of substances between the bloodstream and surrounding tissues. It’s a dynamic and delicate layer that is essential for cell homeostasis—the equilibrium necessary for optimal cell performance and survival.
However, when the delicate balance of the vascular endothelium is disrupted, it can set off a cascade of undesired events, marking the commencement of cellular dysfunction. Studies substantiate the pivotal influence of endothelial health on the onset of atherosclerosis, an insidious type of cell dysfunction that undermines vascular wellness. The associated damage is not solely the result of inherent cellular flaws but is often provoked by external forces like hemodynamics—the physical principles governing blood flow throughout the circulatory system.
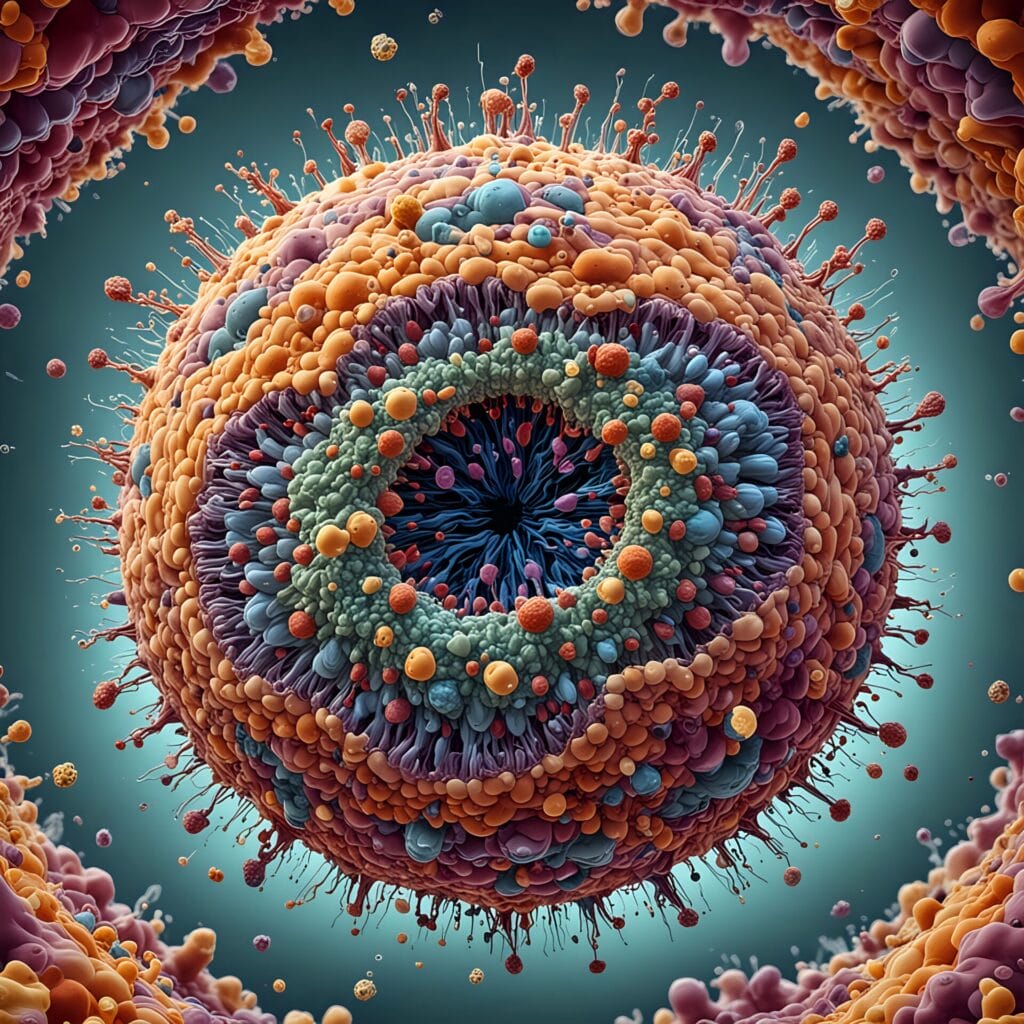
Integrating our understanding, it becomes clear that certain prelesional events, especially the accumulation of cholesterol-rich liposomes within the arterial intima, fuel a hostile environment that is conducive to endothelial injury. This injurious process highlights the significance of fostering environments that promote healthy cellular function. The following image depicts the critical elements involved in maintaining endothelial health and preventing cell dysfunction.
As we delve deeper into the realm of cell biology, it becomes evident that safeguarding cellular health is intrinsically linked to securing our overall well-being. Tending to the fine molecular intricacies that keep our cells in homeostatic harmony not only informs our current medical practices but may also unveil novel strategies to halt or even reverse the progression of debilitating conditions such as atherosclerosis. Through such exploration, we engage in the profound work of preserving life at its most elemental level.
Delineating the Root Causes of Cell Damage
The quest to understand and mitigate cell damage leads us to explore a variety of sources and mechanisms that disrupt the harmony within our cells. Abnormal proliferation of arterial smooth muscle cells, recognized as a hallmark event in the development of atherosclerosis, exemplifies one such source. This uncontrolled growth exemplifies how derangements in cellular behavior contribute to the degradation of vascular health and signify broader issues of cellular dysfunction.
Evidently, the integrity of our cellular systems is predicated on the ability to preserve homeostasis—an equilibrium that, when lost, predisposes our cells to injury and the subsequent interactive turmoil with blood components. This turmoil fosters an environment ripe for cell dysfunction, leading to a range of pathogenic sequelae. It is within this context that the biological imperative for cell regeneration becomes pronounced, as a means to restore normalcy and function.
Ultimately, the effectiveness of cell regeneration mechanisms hinges on detecting and rectifying the root causes of cell damage. Careful examination of these fundamental causes not only sheds light on the pathogenesis of vascular diseases but also offers a window into potential therapeutic interventions. By understanding the underpinnings of these processes, it may be possible to design strategies that enhance the body’s innate ability to heal and regenerate, thereby averting the progression of further dysfunction and its associated aliments.
Highlighting the Impact of Cellular Dysfunction on Overall Health
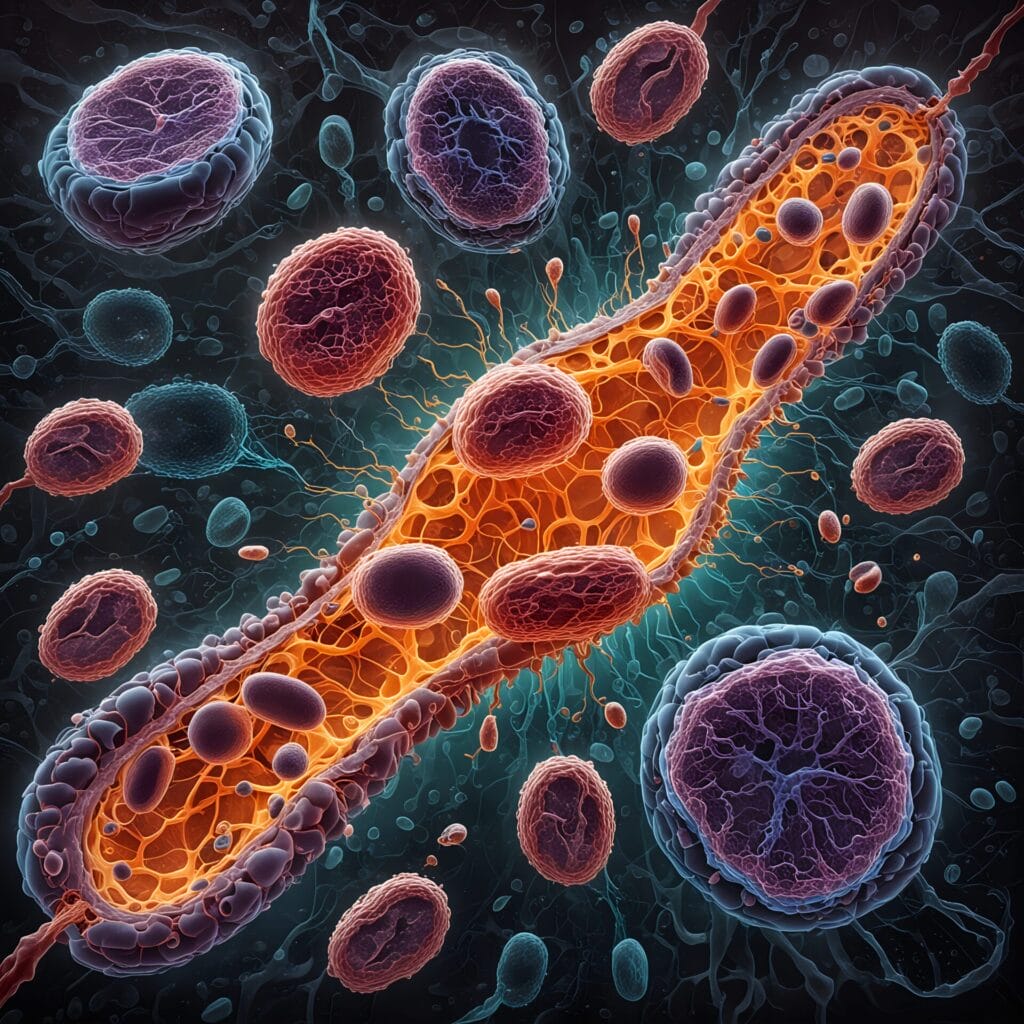
At the cellular level, the vitality and functionality of our organs are deeply interconnected with the state of energy production. A prime factor in this intracellular ecosystem is the health of mitochondria, which are essential for energy generation and overall cellular vitality. The consequences of cell dysfunction is far-reaching, affecting the body’s ability to maintain organ function and resist the ravages of time and disease.
Energy Deficiency and Organ Failure
Cells within high-energy demanding organs such as the heart and brain lean heavily on the internal powerhouses, the mitochondria, to meet their energetic needs. A disruption within these mitochondrial functions can lead to an insufficiency in energy supply, precipitating a cascade of complications that can culminate in organ failure. The deleterious effects of cellular dysfunction in these situations underscore the critical nature of mitochondrial integrity for sustaining life.
Accelerated Aging and Degenerative Diseases
As we age, the efficiency of our cellular processes naturally declines, a decline steeply accelerated by mitochondrial malfunctions. This accelerated aging can manifest in increased susceptibility to a host of degenerative diseases such as Alzheimer’s and Parkinson’s. The cumulative damage incurred over time chips away at the robustness of our cellular systems, highlighting the inevitability of cellular maintenance in promoting longevity and healthy aging.
The Role of Mitochondria in Cellular Vitality
Mitochondria are the linchpins of cellular vitality, and their role transcends mere energy production. Mutations in mitochondrial DNA have been associated with various disorders, further emphasizing the essential nature of these organelles in the context of cell regeneration and overall health. Researchers are continually unraveling the complexities of mitochondrial function to uncover new pathways to combat cell dysfunction and foster cellular repair.
Cellular Dysfunction in Mitochondrial Diseases
Delving into the complexities of mitochondrial diseases offers valuable insights into the nuances of cellular health. These disorders showcase a spectrum of symptoms that are indicative of underlying cell dysfunction. Mitochondrial diseases cause a ripple effect of cellular challenges, such as muscle weakness, intricate neurological issues, and comprehensive metabolic disturbances.
These diseases are a poignant example of how critical the bioenergetic performance of mitochondria is to our cellular well-being. When mitochondria falter, the cell’s ability to generate energy is compromised, leading to a state of compromised cellular health. The consequences of this energy shortfall are profound, influencing not just a single type of cell or system, but potentially affecting every organ and function within the body. As our understanding of these diseases deepens, the interdependence of mitochondrial efficacy and cellular vitality becomes increasingly apparent.
Given that mitochondrial diseases can strike with such diversity in symptomology and severity, they epitomize the central role of mitochondria in maintaining cellular function. From here, the importance of research and therapeutic innovation in this area cannot be overstated; advancements could open doors to not only managing these specific illnesses but also improving broader aspects of cellular health and treating various forms of cell dysfunction.
The Relationship Between Cell Homeostasis and Cellular Function
At the core of cellular vitality and functionality lies the delicate balance of cell homeostasis. The health of each cell, and consequently the health of the entire organism, depends on this stability. This equilibrium is fundamental for sustaining the myriad of biochemical processes that ensure cellular function is optimized.
Within the intricacies of our vascular system, the endothelium exemplifies a complex organ that exemplifies the critical nature of homeostatic balance. By performing a dazzling array of functions, the endothelium serves as a testament to the importance of maintaining cellular health through homeostatic mechanisms.
Understanding Homeostatic Mechanisms in Cells
Homeostasis within cells is achieved through a network of biological checks and balances. These mechanisms continuously monitor and adjust the cellular environment, ensuring that conditions such as pH, temperature, and ion concentrations remain within optimal ranges. Through an intricate dance of molecular signals and responses, cells are able to self-regulate and adapt to changing conditions, thereby preserving the integrity of cellular function.
The Consequences of Homeostatic Disruption
When the balance of cell homeostasis is thrown off, the consequences can be severe. Disruptions can stem from a multitude of sources including genetic mutations, environmental toxins, or inflammatory responses. A failure in homeostasis can trigger cellular dysfunction, leading to cell damage and initiating a chain reaction that compromises the health of the entire organism. As such, it is imperative to understand how homeostatic disruption leads to disease, to develop strategies to prevent or mitigate cellular impairment and maintain cellular health.
Investigating How Cellular Health Influences Disease
The integrity of cellular health is a critical factor in the emergence and progression of various diseases. Within the intricate web of biological systems, the endothelium serves a crucial role in sustaining life. It is the interior surface of blood vessels and is essential for modulating vascular resistance, blood fluidity, and the trafficking of cells and molecules. However, when endothelial cells are compromised, the result can be significant cell damage, which may precipitate a host of diseases.
Consider the endothelium’s responsiveness to stimuli: under normal conditions, a vibrant and dynamic response helps to maintain equilibrium in the bloodstream, ensuring that the tissues it serves are well-nourished and operating at peak efficiency. Nevertheless, when dysfunction occurs—whether due to genetic predispositions, environmental factors, or lifestyle choices—the balance is upended, leading to cell damage and inflammation, key contributors to the pathogenesis of conditions such as atherosclerosis and hypertension.
Thus, the health of each cell has far-reaching implications, stretching beyond their microscopic borders to impact the entire organism. This is where cell repair mechanisms must spring into action, addressing damage and restoring function. Yet, the efficiency of these reparative processes can be diminished by the same variables that harm the cells—creating a challenging cycle of damage and insufficient repair that exacerbates disease.
Embarking on this exploration, we stitch together a clearer picture of just how closely our health is tied to cellular function—demonstrating that preventing and treating diseases largely depend on our ability to foster and maintain robust cellular systems.
In essence, the study of cellular health offers compelling glimpses into the etiology of disease. These biological insights not only enrich our understanding of pathophysiology but also serve as a guiding light for developing innovative treatments that target the cellular underpinnings of illness—treatments that might one day significantly reduce the burden of disease on human health.
Cellular Dysfunction: Triggers and Molecular Pathways
Cellular health is predicated upon a complex and delicate equilibrium, largely orchestrated by signaling pathways that direct the functional operations within a cell. When these pathways falter, they set the stage for cell dysfunction, leading to the onset of cell damage. Understanding the triggers and molecular pathways that underpin cellular health offers a roadmap to mitigate such dysfunction and promote effective cell repair.
Signaling Pathways and the Onset of Dysfunction
Cell signaling pathways are the cellular communication networks that regulate all aspects of cell function, from growth to apoptosis. The integrity of these pathways is essential for maintaining cell health. Disruption in the signaling process can result in cellular dysfunction, which subsequently gives rise to cell damage. Various factors such as genetic mutations, environmental stressors, and toxins can cause distortions in these pathways, necessitating a concerted focus on their regulation to sustain cellular integrity.
Cellular Stress Responses and Dysregulation
Cells possess inherent survival mechanisms known as cellular stress responses. These responses involve a series of adaptive measures taken by the cell to counteract hostile conditions and restore normal function. However, when the stress is excessive or chronic, these protective measures can become dysregulated. Cell dysfunction thus emerges, characterized by a failure in repairing or adapting to the damage. The complexity of cellular stress responses calls for a deepened understanding of their role in cell survival, with an aim to harnessing and enhancing these processes for effective cell repair and regeneration.
Analyzing the Role of Endothelial Cells in Cellular Dysfunction
The linchpin of vascular integrity and overall cell health is the endothelial cell—a dynamic and versatile player in the cardiovascular domain. With their strategic location lining the entire circulatory system, endothelial cells are pivotal in the preservation of cellular function and protection against vascular diseases. As regulators of vascular tone and barriers to inflammatory and coagulatory triggers, these cells orchestrate a wide range of critical physiological responses that maintain homeostasis within the body’s intricate networks.
Alterations in endothelial cell morphology—an observable manifestation of cellular dysfunction—serve as indicators of the cell’s struggle to maintain this homeostatic balance. Phenomena such as endothelial activation or endothelial senescence not only reflect immediate distress but also potentially foreshadow long-term compromisation of vascular function. Moreover, the rate of endothelial turnover provides invaluable insights into the cell’s resilience and capacity for repair, which can directly impact the progression of vascular ailments.
Moreover, research underscores the relationship between cell dysfunction and systemic diseases. Endothelial dysfunction, often marked by a proatherogenic phenotype, includes aberrant expression of adhesion molecules and reduced nitric oxide bioavailability, both of which herald the onset of pathologic conditions like atherosclerosis—an archetypal disease process stemming from compromised cellular health.
Ultimately, the integrity of endothelial cells serves as a gauge for the broader state of cell health. Their ability to respond adequately to physiological stimuli is an essential determinant of vascular responsiveness and disease susceptibility. As scientific inquiry delves deeper into endothelial cell biology, it lays the foundation for developing novel diagnostic markers and therapeutic targets aimed at combating the insidious nature of cellular dysfunction.
The Intricacies of Cell Repair and Regeneration
The ecosystem of the human body is sustained by the remarkable ability for cell repair and regenerative capacity, pivotal for maintaining cellular health. This intricate process is critical for recovery from injury and for the normal wear and tear of daily life. At the core of this regenerative prowess are the cells’ multifaceted mechanisms geared toward repair and renewal.
Mechanisms of Cellular Repair
When cellular integrity is compromised, the body initiates a series of complex biochemical events to restore function. One such mechanism involves endothelial regeneration, a process by which the lining of our blood vessels repairs itself after injury. This regenerative process is integral to cardiovascular health and is mediated by the synthesis of crucial compounds, such as prostaglandins, which play a pivotal role in vascular repair and homeostasis. The intricate interactions of these mechanisms not only highlight the sophistication of cellular health systems but also underscore the importance of ensuring these pathways are unobstructed and functional.
Factors Affecting Regenerative Capacity
However, the body’s ability to conduct cell repair and encourage cellular regeneration is not constant and can be affected by various factors. Genetic mutations may alter the normal repair functions of cells, leading to inadequate or faulty regenerative processes. Environmental toxins can also impede cellular repair mechanisms, resulting in a diminished regenerative capacity. Recognizing and understanding these variables is paramount for developing effective treatment strategies aimed at enhancing cellular health and mitigating disease progression.
Advances in cellular health, focused on optimizing repair and regeneration capabilities, hold great promise for improving treatment outcomes in diseases where cell dysfunction plays a fundamental role. The scientific and medical communities continue to explore these remarkable biological processes, aiming to harness their full potential to enhance human health.
Uncovering the Effects of Environmental Toxins on Cells
The silent yet pervasive presence of environmental toxins in our surroundings poses a formidable threat to cellular health, often catalyzing cellular dysfunction and the subsequent cellular damage. These toxins, ubiquitous in air, water, and soil, can originate from industrial emissions, agricultural chemicals, and even household products. Sadly, their insidious influence extends to the very building blocks of life—our cells—where they disrupt critical biological processes essential for cell vitality and function.
Our cells’ interface with the environment means they are perennially at risk of exposure to harmful agents. When toxins infiltrate these biological systems, they can induce oxidative stress, a process that accelerates cell damage and contributes to cellular dysfunction. The accumulation of such damage can compromise the cell’s ability to repair itself, leading to a decline in overall cellular function and health.
To combat this threat, the development and implementation of detoxifying strategies are of paramount importance. Key to these methods is the reduction of toxin exposure, which involves both societal changes, such as stricter pollution controls, and personal choices, such as opting for organic produce or toxin-free home products. Moreover, supporting the body’s natural detoxification pathways, through nutrition and lifestyle adjustments, serves as an essential aid in fortifying cellular resilience against the onslaught of environmental pollutants.
While research continues to elucidate the full impact of environmental toxins on cellular health, it’s clear that the stakes are high. The quest to shield our cells from such detrimental exposures and promote effective cell repair is more than a scientific challenge—it’s a crucial endeavor for safeguarding human health against the backdrop of an increasingly contaminated world.
Genetic Mutations and Their Influence on Cellular Dysfunction
Within the intricate web of hereditary factors lies the blueprint of our health, where the delicate equilibrium of cell process can be destabilized by genetic mutations. These mutations are significant contributors to cell dysfunction and serve as a central focus of scientific inquiry into the genesis and progression of various diseases. Unpacking the genetic underpinnings of cell health is not only pivotal for understanding the breadth of disease prevalence but also for tailoring individualized treatment options.
Hereditary Factors and Disease Prevalence
Overwhelming evidence underscores that hereditary factors can greatly influence the likelihood of developing certain conditions. Genetic mutations, particularly those impacting mitochondrial DNA and nuclear DNA, are instrumental in such predispositions. As carriers of hereditary information, these two types of DNA encode for necessary components of cellular function. The dysfunction arising from mutations within them can lend insight into the prevalence and heterogeneity of diseases at both individual and population levels.
Tracking Mutations in Mitochondrial and Nuclear DNA
The symbiotic relationship between mitochondrial DNA and nuclear DNA is nothing short of a complex masterpiece in the realm of genetic research. Detecting genetic mutations in these DNA types is crucial for understanding the multifaceted nature of cellular dysfunction. Indeed, mitochondrial DNA—responsible for a host of cellular energy processes—when altered, can precipitate systemic cell dysfunction. Conversely, mutations in nuclear DNA can disrupt the integrity of a wide array of cellular operations. The tracking and analysis of these genetic abnormalities play a crucial role in the advancement of molecular medicine and the formulation of targeted therapies that aim to restore cellular health.
Understanding the Complex Interplay Between Cellular Dysfunction and Aging
The intertwining relationship between cell dysfunction and the natural progression of aging goes beyond the mere ticking of our biological clocks. As we delve into the cellular domain, we uncover how processes like cellular senescence and oxidative stress underscore the gradual deterioration of cellular function—a pivotal factor in the onset of age-related conditions. This intricate dance between cellular stability and the inevitable march of time accentuates the need for a thorough exploration into the molecular pathways that govern aging cells.
How Cellular Senescence Contributes to Aging
A term that’s becoming increasingly synonymous with aging in the scientific community is cellular senescence. It describes the cessation of cell division—a process once vital to growth and healing—turned detrimental as cells stagnate and accrue in our bodies. This state not only halts the regenerative potential of tissues but also emits inflammatory signals that further perpetuate the cycle of cellular dysfunction. These senescent cells are like the aged gears of a machine, still present but no longer contributing to the system’s efficiency, thereby contributing to the broader spectrum of aging.
The Effects of Oxidative Stress on Aging Cells
Compounding the effects of cellular senescence is oxidative stress—a relentless force that accelerates the decline of aging cells. The very byproducts of our cellular respiration, reactive oxygen species (ROS), accumulate over the decades, inflicting damage on DNA, proteins, and lipids. This cumulative oxidative havoc impairs critical cellular functions, rendering once-vibrant cells sluggish and susceptible to a multitude of aging-related pathologies. As research delves deeper into combating oxidative stress, we gain valuable ground in our efforts to preserve cellular function and retard the aging process.
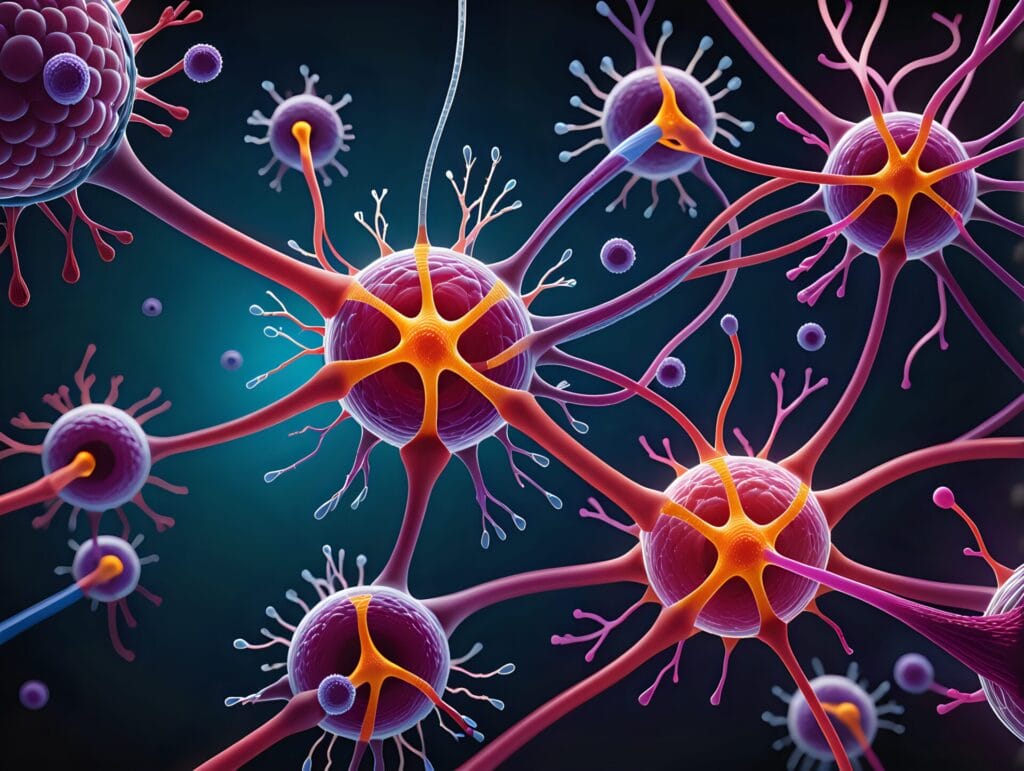
Neurological Impacts of Cellular Dysfunction
The consequences of cell dysfunction on neurological health constitute a critical area of research due to the profound implications for human well-being. Cells within the nervous system require meticulous regulation and coordination to function correctly. Disruption to this system can precipitate severe neurological impacts, including seizures, cognitive impairments, and an array of neurodegenerative diseases.
Within the brain, neuronal cells heavily rely on a consistent and high-quality energy supply to maintain their complex operations. When energy production within these cells is compromised due to mitochondrial abnormalities or other causes of cell dysfunction, the effects can be particularly devastating. Inadequate energy provision can lead to cell damage, and in the highly specialized and interconnected environment of the brain, this damage can disrupt neural pathways, altering cognitive and functional abilities.
Numerous studies have linked this dysfunction to a spectrum of neurological disorders, highlighting the crucial role that cell health plays in maintaining neurological function. Conditions such as Alzheimer’s and Parkinson’s diseases have been intimately associated with the degeneration of cellular mechanisms, reiterating the importance of ensuring cellular resilience and vitality in neurology.
The identification of early markers of cellular dysfunction within the nervous system could pave the way for preventative measures against future neurological impacts. Moreover, novel interventions designed to protect or restore cellular health present promising avenues for mitigating the burdens of these dysfunctions. As scientists continue to unravel the mysteries of cellular processes, their findings will be instrumental in shaping the future of neurological healthcare and therapy.
The Role of Cellular Vitality in Metabolic Disorders
As the cornerstone of health, cellular vitality plays a pivotal role in the body’s overall metabolic function. The integrity of cellular processes is often reflected in the efficiency of energy metabolism, and it is in this domain that many metabolic disorders find their origin. With energy production at the heart of cellular activity, disruptions within this realm can have profound implications for the emergence and progression of various metabolic diseases.
Disrupted Energy Metabolism and Metabolic Diseases
A clear illustration of the consequences of compromised cellular health is observed in the landscape of metabolic disorders. These ailments, characterized by an imbalance in the production and utilization of energy within cells, underscore the delicate balance required for optimal cell function. When cells falter in their role as energy producers, the body becomes predisposed to a range of disorders that manifest as systemic health issues, directly tethered to the concept of cellular vitality.
Insights into Diabetes and Cellular Health
One cannot discuss metabolic disorders without considering diabetes—an emblematic condition marked by chronic cell dysfunction and aberrant metabolic processes. At the crux of diabetes is a discordance between insulin action and glucose management, a reflection of impaired cellular machinery. Diabetes is thus not just a disease of blood glucose levels; it is a signal of deeper disturbances in cellular vitality. For individuals living with this condition, targeting the roots of cellular dysfunction can hold the key to more effective treatments and a better understanding of cellular health at large.
Utilizing a natural supplements based glutathione precursor protocol like our Viprox Therapy can greatly enhance your over all health. The Viprox Protocol consists of Viprox and Viprox Junior packages. The packages contain GSH Complex for restoring, strengthening and balancing your immune system. Une Vie for enhanced hydration and Triozyme enzymes that support improved digestion.
- Glutathione for Hangovers: Your Recovery Solution - July 2, 2024
- Top Glutathione Foods High in Antioxidant Power - June 30, 2024
- Boost Your Health with Top Foods for Glutathione - June 21, 2024